Our Partners
At Active Path, we have partnered with the leading TMS manufacturers, including NeuroStar Advanced Therapy and BrainsWay, to bring the latest in technology to our patients. This means we can offer several types of TMS treatment: BrainsWay’s dTMS and NeuroStar Advanced Therapy.
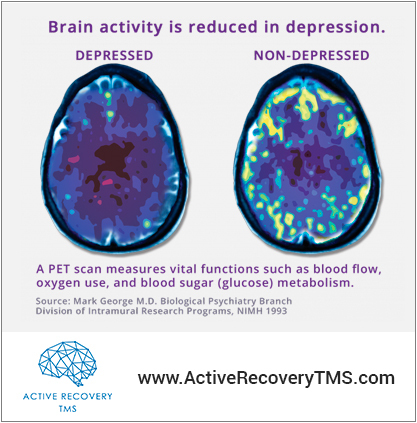
With Deep TMS (dTMS) magnetic pulses travel more deeply, allowing the therapy to stimulate more parts of the brain and provide broader stimulation of the targeted region of the brain involved in MDD, the dorsolateral prefrontal cortex. NeuroStar’s rTMS treatment protocol has recently been redesigned to reduce treatment time to just under 20 minutes with some variation from patient to patient. To read more about this technology, visit our Device Partners page.